Attention-deficit/hyperactivity disorder (ADHD) is one of the most common neurological disorders affecting children with an estimated prevalence of 6.7% to 12% in the United States. The current research indicates that about half of those diagnosed with the disorder will carry their symptoms into adulthood.
Fortunately, the literature also contains plenty of clues as to how we can potentially alleviate many of the symptoms of ADHD naturally. In this article, we will focus on natural treatments for ADHD, specifically dietary interventions like the ketogenic diet.
What is ADHD?
Do you find it hard to pay attention? Do you feel the need to move continuously when you should be calm and relaxed? Do you find yourself constantly interrupting others?
These are the most commonly known characteristics of ADHD, but the disorder, as a whole, is much more complicated than simply struggling to stay focused and calm.
In general, ADHD is characterized by a lack of behavioral regulation and by neurological deficits in four areas, including working memory, self-regulation of emotions, internalization of speech, and behavioral analysis and synthesis.
Because of how nuanced the characteristics of ADHD are, the disorder is typically broken down further into three main types: inattentive type, hyperactive/impulsive type, or combined type.
Inattentive type – when six (or five for people over 17 years) of the following symptoms occur frequently:
- Struggle with paying attention to detail and makes careless mistakes.
- Has problems staying focused on tasks or activities, like lectures, homework, and conversations.
- Does not seem to listen when being spoken to.
- Does not follow through on instructions and doesn’t complete schoolwork, chores, or job duties (may start tasks but quickly loses focus).
- Does not manage time well, has messy, disorganized work, and misses deadlines.
- Avoids or dislikes tasks that require sustained mental effort.
- Often loses important things, such as school papers, books, keys, wallet, cell phone, and eyeglasses.
- Is easily distracted.
- Forgets to pay bills or do daily tasks, such as doing chores and running errands.
Hyperactive/impulsive type – when six (or five for people over 17 years) of the following symptoms occur frequently:
- Fidgets and/or squirms constantly when seated.
- Not able to stay seated when necessary.
- Runs about or climbs where it is inappropriate.
- Unable to play or do leisure activities quietly.
- Always “on the go” or active.
- Talks more than is necessary.
- Talks while other people are talking.
- Has difficulty waiting for things, such as standing in line.
- Interrupts or intrudes on others without permission. Older teens and adults may take over what others are doing without asking.
There is no lab test to diagnose ADHD. Diagnosis involves gathering information from parents, teachers, and others, filling out checklists and having a medical evaluation (including vision and hearing screening) to rule out other medical problems.
It is also important to note that these symptoms are not the result of the person being defiant, hostile, or unable to understand a task or instructions. The symptoms of ADHD are the outward expression of multiple modifiable and non-modifiable factors that disrupt the proper functioning of the brain.
The Cause of ADHD
ADHD is one of the most researched and written about neurological disorders of childhood and adolescence and so is the treatment of ADHD, but the exact cause is still uncertain.
Current evidence suggests that the cause of ADHD is multifactorial, and both genetic and environmental factors are involved in its development. Let’s take a closer look at the variables that we know play a role in the disorder:
- Genetics. Three out of four children with ADHD have a relative with the disorder, indicating that genetic inheritance may play a role in ADHD. The current research is inconclusive, but genetic studies do suggest the involvement of genes related to the receptors and transporters of dopamine and serotonin, two neurotransmitters that help regulate behavior.
- Gestational stressors. Being born prematurely and the mother smoking, using alcohol, or experiencing extreme stress during pregnancy are all associated with the development of ADHD.
- Childhood trauma. Whether it is a physical injury like brain injury or emotional abuse, childhood trauma can provoke many of the symptoms of ADHD.
- Toxin exposure. Heavy metal and chemical exposures such as lead, mercury, organochlorine, organophosphates, and phthalates can all negatively impact brain development (in both the fetus and the child) that may cause ADHD.
- Diet. The effect of diet and dietary supplements is unclear, but considerable evidence suggests that nutritional factors are associated with ADHD. For example, low levels of copper, iron, zinc, magnesium, and omega-3 fatty acids are commonly found in children with ADHD, and sugar, artificial food colorings, and preservatives are associated with an increased risk of ADHD.
This is not a comprehensive list of all the factors that contribute to the formation and progression of ADHD — and the cause is far from being known. However, the current literature does provide us with clues to the most effective long-term treatment strategy.
Natural Treatments for ADHD
Although the first line of treatment is typically stimulants (e.g., Adderall and Ritalin) , the therapeutic approach to ADHD has been shifting. In some cases, environmental changes and behavioral therapy alone are helpful enough.
With that being said, studies have found that a combination of behavioral therapy and medication works best for most people, particularly those with moderate to severe ADHD. However, there are other natural treatment options worth exploring for those who do not respond to medication or who don’t want to rely on ADHD drugs.
Let’s take a look at the most common natural, drug-free ADHD treatments that address multiple potential causes of the condition:
Behavioral Therapy, Education, and Training
There are different kinds of therapy that have been used for ADHD, but research has found that therapy alone is not effective at reducing ADHD symptoms. This is in part due to the neurological issues that are driven by other variables.
Therapy is best used as a supplement to an ADHD treatment plan, as a way to help the children, teens, and adults with the disorder work through common issues instead of avoiding them.
For example, therapy for children and teens may look like this:
Parents and teachers are taught how to help children and teens with ADHD stay organized and follow directions with tools such as keeping a routine and a schedule, organizing everyday items, using homework and notebook organizers, and giving praise or rewards when rules are followed.
And therapy for adults may look something like this:
A licensed mental health provider or therapist can help an adult with ADHD learn how to organize his or her life with tools such as keeping routines and breaking down large tasks into more manageable, smaller tasks.
Another crucial part of the treatment process is understanding ADHD and how to work with the symptoms. This will require diligent education and training of children and adults with ADHD as well as their parents, families, and teachers.
To do this, mental health professionals will be enlisted to educate the parents of a child with ADHD about the condition and how it affects a family. They can also help the child and his or her parents develop new skills, attitudes, stress management techniques, and ways of relating to each other.
Altogether, behavioral therapy, counseling, and practical support can play a helpful role in managing the disorder, but these approaches won’t address the underlying causes and help alleviate symptoms of ADHD like the remaining three strategies have been found to do.
Addressing Nutrient Deficiencies
Chronic deficiencies of certain minerals such as zinc, iron, magnesium and iodine and inadequate dietary intake of omega-3s may have a significant impact on the development and progression of the symptoms of ADHD in children. By addressing these deficiencies, it is possible to improve brain function and potentially reduce some symptoms of ADHD.
The best way to address these deficiencies is with a micronutrient-dense diet consisting of whole foods that the patient can tolerate. Some examples of these vitamin- and mineral-rich foods include seafood, seaweed, organ meats, low-carb vegetables, and egg yolks. However, if these foods are not tolerated by the patient (i.e., they are sensitive or have an allergic reaction to it), then supplements are the next best option.
Supplements
Although there are many proposed ADHD “remedies” available, the evidence for their effectiveness is virtually nonexistent. At this point, only three supplemental strategies have relatively high-quality research supporting their effectiveness for those affected by ADHD:
- Omega 3s (DHA and EPA). The most recent systematic reviews and meta-analyses of the studies assessing the impact of omega 3s on ADHD symptoms conclude that these fatty acids have a modest positive effect. Researchers recommend that the use of omega-3 fatty acids in the treatment of ADHD should generally be reserved for mild cases and as a supplemental treatment in more severe ADHD cases.
- Melatonin. Melatonin appears to be an excellent option for treating sleep problems (stimulant-induced or not), especially if behavioral treatments have been unsuccessful and reducing or adjusting medication dosages is not feasible.
- Vitamin and minerals that are deficient in the diet. Ensuring adequate micronutrient intake is a crucial part of optimizing cognitive function, especially for those vulnerable to ADHD symptoms.
Dietary Interventions

According to the research, dietary interventions seem to help roughly one in every four children with ADHD. The minority of these individuals — around 10% of children with ADHD — may experience a full remission of symptoms that is equivalent to a successful drug treatment.
Among all of the “ADHD diets” studied, the “few foods diet” seems to be most effective. Simply put, this diet restricts a person’s calories to only a few less commonly consumed foods (eg, lamb/venison, rice, pear, peas, and others with low allergenic potential).
It also eliminates many of the foods and food ingredients that may trigger ADHD symptoms, such as:
- artificial colorings, such as red 40 and yellow 5
- artificial flavorings, such as synthetic vanilla
- artificial sweeteners, such as aspartame, saccharin, and sucralose
- chemicals naturally found in some foods, such as salicylates found in apricots, berries, and tomatoes
- preservatives, such as butylated hydroxyanisole (BHA), butylated hydroxytoluene (BHT), andtert-Butylhydroquinone (TBHQ)
- butylated hydroxyanisole and Butylated hydroxytoluene
- carrageenan
- monosodium or monopotassium glutamate
- any hydrolyzed, textured, or modified protein
- added sugars
- high glycemic foods
- any food allergens or sensitivities
Although this diet is the most restrictive of the diets proposed to help those with ADHD, it is highly effective for many reasons:
- It reduces the person’s toxic load.
- It prevents allergic reactions and food sensitivities.
- It decreases sugar intake.
By possessing these qualities, the few foods diet addresses many potential causes of ADHD symptoms. However, this highly restrictive comes with the increased risk of nutrient deficiency, so it must be overseen by a properly qualified professional (e.g., dietitian) to ensure optimal health.
If the few foods diet is not feasible, then your next best option is to limit the intake of the foods and food ingredients from the above list. This approach is a bit less restrictive, but it still has the potential to help alleviate some ADHD symptoms.
Another dietary intervention worth exploring for ADHD treatment is the keto diet. It serves as a pseudo-elimination diet that mimics many characteristics of the few foods diets while stimulating further positive changes throughout the brain with the help of ketones.
The Ketogenic Diet and ADHD
The ketogenic diet has a long-standing place in neurology which was first used to help children with treatment-resistant epilepsy in the 1920s. Since then, keto has been proven effective as a treatment for various cases of epilepsy.
There is also a plethora of research indicating that keto dieting can help improve the function of dysfunctional metabolic pathways involved in some neurological disorders including autism spectrum disorder, Parkinson’s disease, and Alzheimer’s disease.
Interestingly enough, many of these conditions share similarities with ADHD. Does this mean that keto can help patients with ADHD as well?
Unfortunately, the research on keto and ADHD is scarce. In fact, the highest quality research I could find was conducted on dogs, not humans.
Regardless, the data can still provide us with some valuable insights into how carb restriction may impact ADHD-related behaviors. In this 6-month dietary trial, 21 dogs that had both ADHD and idiopathic epilepsy were put on either a keto diet or a standard diet.
When compared with the standard diet, the keto diet resulted in a significant improvement in ADHD-related behaviors, which are similar to behaviors expressed by humans with the condition.
The authors speculated that the alterations of energy metabolism in the brain — a phenomenon that occurs after the body starts burning more ketones for fuel — may have contributed to the behavioral changes. Hopefully, these promising results will provoke more of a demand for high-quality trials of the keto diet or ketone supplementation as a potential dietary intervention for ADHD in humans.
Why Keto May Be Helpful for ADHD
In short, keto dieting is worth exploring as a potential treatment strategy for patients with ADHD because it eliminates many of the unhealthy ingredients that may worsen ADHD-related symptoms while simultaneously stimulating ketone production.
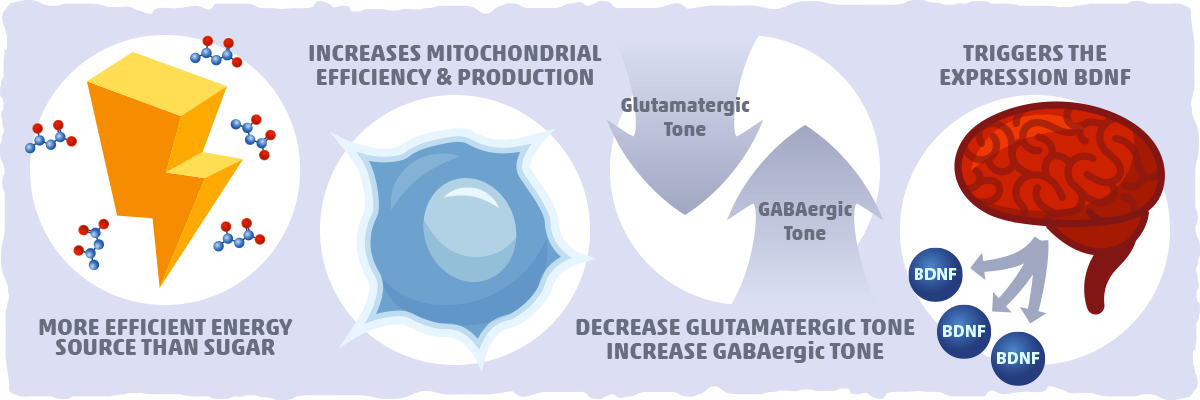
When our brain starts burning more ketones for fuel, it causes a cascade of effects that may alleviate many ADHD-related symptoms. Let’s take a quick look at how ketones may be able to do this:
- Ketones are a more efficient energy source than sugar. Ketone bodies (beta-hydroxybutyrate, in particular) are a more efficient source of energy per unit oxygen than glucose. In other words, by using ketones for fuel, your nerve cells will be able to do their job in a way that doesn’t cause excess damage.
- Ketones increase mitochondrial efficiency and production. The ketogenic diet induces a coordinated up-regulation of mitochondrial genes and genes involved in energy metabolism while stimulating the biogenesis of mitochondria. Altogether, this enhances the capacity of brain cells, protecting them from the metabolic dysfunction that can provoke ADHD-related symptoms.
- Ketones increase GABAergic tone and decrease glutamatergic tone. Glutamate, the brain’s primary excitatory neurotransmitter, is the precursor for GABA, the brain’s main inhibitory neurotransmitter. Glutamate is essential for neural communication, memory formation, learning, and regulation, but under certain conditions, glutamate can damage or kill nerve cells. This may be a contributing factor to some of the symptoms of ADHD. Although the mechanisms are unclear, ketones have been found to decrease glutamatergic tone and increase GABAergic tone, which helps prevent brain cell damage and improve function.
- Ketones trigger the expression BDNF. BDNF or Brain-derived neurotrophic factor is a protein that helps stimulate growth and proliferation for specific neurons throughout the nervous system. Ketones have been found to trigger the expression of BDNF in ways that can improve the function of the hippocampus, cortex, and basal forebrain — areas of the brain that play a vital role in learning, memory, and higher thinking. From a practical perspective, this indicates that the combination of behavioral therapy and ketone burning may be an effective treatment strategy for some cases of ADHD.
Although the keto diet can provide you with all of these benefits, it may also provoke a negative reaction if the ADHD symptoms are related to allergies and intolerances to common keto-friendly foods. For this reason, you may need to experiment with different dietary strategies and natural treatments to see what works best for you or your loved one with ADHD. To help you formulate a natural treatment plan with your doctor, let’s finish this article with the key aspects of an ADHD diet.
What Would a Keto ADHD Diet Look Like? List of Foods to Eat, Limit, and Avoid
Putting the above information into practice can be a confusing and overwhelming task, so we distilled it down to its critical components in the following food list.
This will give you a better idea of what foods to focus on and what to avoid when formulating a keto-friendly ADHD diet.
What to Eat
- Fresh meat – beef, lamb, poultry, etc.
- Eggs — pasture-raised whole eggs are best.
- Fatty fish/seafood — low-mercury sustainably-caught salmon, mackerel, sardines, etc.
- Low-carb vegetables – broccoli, cauliflower, spinach, and other low-carb veggies
- High-fat dairy – hard cheeses, full-fat cream, butter, and other keto dairy products
- Nuts and seeds – macadamias, walnuts, sunflower seeds, and other low-carb options
- Low-carb fruit – avocado, tomato, olives, berries, and other low-carb fruits
- Natural keto sweeteners – stevia, erythritol, monk fruit, and other low-carb sweeteners
- Other fats – MCT oil, coconut oil, high-fat salad dressing, keto mayo, etc.
However, there may be some keto-friendly foods that trigger symptoms as well. If you’d like to try a more restricted elimination diet, consider avoiding one or more of the following foods for a few weeks to see if symptoms improve.
Keto foods that might trigger symptoms
- High-salicylate foods — Tomatoes, berries, broccoli, and zucchini are some examples of high-salicylate foods that may trigger symptoms.
- Dairy — Many of us are either sensitive to proteins in dairy, allergic to dairy, or lactose intolerant. For more information on how to limit dairy intake, check out our comprehensive guide to dairy-free keto.
- Other common food allergies and sensitivities — Eggs, tree nuts, peanuts, shellfish, and fish are common culprits to consider as well.
List of Foods to Avoid
- Heavily processed food products — As a general rule of thumb, if it doesn’t consist of real food ingredients, then it is best to avoid it. This helps ensure that you are avoiding the artificial flavors, dyes, and other chemicals that may trigger hyperactivity.
- Added sugars – honey, agave, maple syrup, cane syrup, etc.
- Fruit and fruit juice – apples, bananas, oranges, etc.
- Starchy tubers – potato, yams, cassava, etc.
- Beans and legumes — lentils, black beans, soybeans, etc.
- Grains and grain-based foods – wheat, corn, rice, cereal, bread, pastries, etc.
Avoiding these foods will help reduce the overall intake of sugar, high GI foods, artificial ingredients, potential allergens, and food sensitivities significantly. This list may be all you need to enter nutritional ketosis and reap the benefits of keto as well.
That being said, make sure to consult a physician to help test and address any nutritional deficiencies that already exist or may arise after making these dietary changes. Additional supplementation may be necessary to ensure adequate nutrition.
What Would a Keto Meal Plan for ADHD Look Like? Tasty Low Carb Recipes for Breakfast, Lunch, Dinner, and Dessert
Before we bring this article to a close, let’s explore some nutritious and delicious keto recipes we can use to help transition away from an unhealthy diet filled with processed foods.
Make sure to read the ingredients carefully, as many of the following recipes contain low-carb foods you may be trying to limit. We’ve included allergen-free ingredient substitutions and tips where possible.
Sugar-free Breakfast Recipes
Keto Granola Cereal — Skip the sugary cereal, and try this healthy keto alternative instead. Use the flavor tips and ingredient substitutions on the recipe page to adjust your cereal recipe as needed.
Dairy-Free Dark Chocolate Shake — This recipe has the mouthfeel and flavor of a rich chocolate milkshake but is packed with a surprising amount of guilt-free nutrition. Perfect for anyone who is lactose intolerant, allergic to dairy, or sensitive to specific dairy proteins.
Peanut Butter Pancakes — Keto-friendly pancakes that are just like the real thing! Although they contain several common food allergens, this recipe is easy to adjust to your dietary preferences. For example, you can replace the heavy cream with coconut cream to make them dairy-free, use an egg alternative to go egg-free, or substitute peanut butter for sunflower seed butter for a pancake that is nut-free and peanut-free.
Healthy Lunch Ideas for the Picky Eater
5-min Personal Keto Pizza — Low-carb, gluten-free pizza that is ready in 5 minutes and easy-to-make.
Low Carb Zesty Chicken Nuggets — Finding delicious nuggets without dubious ingredients is nearly impossible. Your best bet for making this comfort food healthy and delicious is with this keto recipe. Feel free to adjust the spices as needed.
Keto Coconut Curry Chicken Tenders — Our keto-friendly adaptation of children’s menu chicken fingers but much healthier. If you prefer to make them plain (without the curry flavor), just stick with the first four ingredients and your desired seasonings.
Easy-to-pack Sugar-free Snack Ideas
Snacks are typically filled with unhealthy ingredients that can trigger symptoms. For this reason, popular store-bought snacks — such as fruit rollups, fruit snacks, chips, cheez-its, and goldfish — should be avoided.
Here are some of the best sugar-free alternatives for those high-carb culprits:
If you would rather find some grab-and-go keto snacks that you don’t have to make, check out our healthy snack list.
Simple Dinner Entree Ideas
Chicken Tender Lazone — A flavorful, comforting chicken entree that provides us with a delicious way to sneak in some extra keto vegetables.
Keto Salmon Meatballs with Lemon Sauce — Packed with low-carb veggies and omega-3 fatty acids, these meatballs are perfect for anyone who isn’t fond of fish.
Cauliflower Pizza Crust — Make pizza for the whole family with the help of keto cauliflower crust. This crust is so good that you’ll forget that it’s made out of veggies.
Healthy Keto Desserts
Keto Avocado Brownies — These rich, satisfying brownies are packed with nutrition and easy-to-make. Check out the recipe page for ingredient substitutions and links to other brownie recipes for keto.
Keto Chocolate Chunk Cookies — Sugar-free cookies with all the flavors and textures we crave from these delicious little delicacies. For more sugar-free options, take a look at our top 10 keto cookie recipes.
Chocolate Chunk Avocado Ice Cream — Who said ice cream couldn’t be healthy, delicious, and sugar-free? Give this recipe a try, especially if you need something to satisfy your sweet tooth.
Putting It All Together — The Key Aspects of an ADHD Diet
Although the data on how different dietary approaches affect patients with ADHD is inconclusive, there are a few strategies that have the potential to help:
- Eliminate all dubious food additives that the person may be sensitive to (i.e., artificial colorings, flavorings, sweeteners, and preservatives).
- Limit added sugar and high GI food intake.
- Remove all foods that the person is allergic or sensitive to.
- Stimulate ketone production with a keto diet and/or supplement with ketone-boosting supplements (i.e., MCT oil).
- Address any vitamin and mineral deficiencies with micronutrient dense foods and/or supplements. (check out this article if you’d like to learn more about micronutrients.)
- Use science-backed supplements, such as fish oil, melatonin, or zinc, when necessary.
At this point, the research on ADHD indicates that these are the qualities that the ideal ADHD diet should have. By following these guidelines, many (if not all) of the symptoms of ADHD can be reversed or at least reduced in those who have a dietary component to their symptoms.
With that being said, the research on dietary interventions and supplementation for ADHD is still sparse, so it is best not to use these recommendations as a replacement for other common treatments like ADHD medications and behavioral therapy.
The best ADHD treatment plan will consist of the medications, therapies, and/or dietary strategies that apply to each individual’s specific needs.
Sources:
- Autism and the Ketogenic Diet — Ruled.me
- Ketones And The Brain: The Unique Benefits of Keto — Ruled.me
- Diet in the treatment of ADHD in children—A systematic review of the literature — Nordic Journal of Psychiatry
- Dietary Patterns in Children with Attention Deficit/Hyperactivity Disorder (ADHD) — NCBI
- The Current Status of the Ketogenic Diet in Psychiatry — NCBI
- Attention-Deficit/Hyperactivity Disorder (ADHD): The Basics — NIH
- Restriction and Elimination Diets in ADHD Treatment — NCBI
- The diet factor in attention-deficit/hyperactivity disorder. — NCBI
- Nutritional Supplements for the Treatment of Attention-Deficit Hyperactivity Disorder — NCBI
- The influence of components of diet on the symptoms of ADHD in children. — NCBI
- The ADHD Diet: What Works, What Doesn’t — Healthline
- Pharmacological Treatment of Attention Deficit Hyperactivity Disorder in Children and Adolescents: Clinical Strategies — NCBI
- Diet and ADHD, Reviewing the Evidence: A Systematic Review of Meta-Analyses of Double-Blind Placebo-Controlled Trials Evaluating the Efficacy of Diet Interventions on the Behavior of Children with ADHD — NCBI
- Impulsivity and Aggression in Female BPD and ADHD Patients: Association with ACC Glutamate and GABA Concentrations — NCBI
- Glutamatergic and GABAergic gene sets in attention-deficit/hyperactivity disorder: association to overlapping traits in ADHD and autism — NCBI
- Brain Balance — Science-Based Medicine