Alzheimer’s disease is the most prevalent neurodegenerative disease and the leading cause of dementia. For decades, researchers have been struggling to find therapies that prevent or, at least, delay the progression of the disease, but now we have some promising evidence.
Current research suggests that the ketogenic diet and ketones have a wide range of neurological benefits that help address many factors that contribute to the progression of Alzheimer’s disease. However, before we get into the potential that the ketogenic diet and ketones hold as an Alzheimer’s treatment (and — dare I say — as a possible cure), let’s get a better understanding of the disease first.
What Is Alzheimer’s Disease?
Alzheimer’s disease was first discovered by Dr. Alois Alzheimer, who observed a woman with symptoms of the disease in 1906 and examined her brain after she passed away. During the examination, Dr. Alzheimer found that the woman’s brain contained many strange clumps and fiber tangles.
Today, we refer to these unusual clumps as beta-amyloid plaque and strange fiber tangles as neurofibrillary tangles. Each one interferes with neuronal connections and brain cell function, which causes thinking and memory abilities to decline. As the tangles and plaque accumulate in the brain, the symptoms get worse, and the patient moves to more advanced stages of Alzheimer’s disease.
Although the beta-amyloid plaque and neurofibrillary tangles can start accumulating before old age, the first Alzheimer’s symptoms will usually show up in a person’s mid-60s if they have the disease. Because the disease tends to progress stealthily with very subtle signs at first, many scientists are focused on finding ways to identify the disease in its earliest stages. By diagnosing the disease before memory loss takes hold, we have a higher likelihood of stopping its progression and reversing some aspects of the disease. At this point, however, there is no legitimate cure — even if Alzheimer’s disease is diagnosed in its early stages.
Alzheimer’s Disease Stages
Stage 1: No Signs or Symptoms
This is the stage where we want to detect the disease for the best possible treatment outcomes. During this phase, Alzheimer’s disease is not detectable, and no memory problems or other symptoms are evident.
Stage 2: Minor Memory Issues
The patient may notice minor memory problems or lose things around the house, although not to the point where the memory loss can easily be distinguished from normal age-related memory loss.
Stage 3: Mild Decline
At this stage, the friends and family members of the patient may begin to notice memory and cognitive problems.
Patients in stage 3 will have difficulty in many areas including:
- Finding the right word during conversations
- Remembering names of new acquaintances
- Planning and organizing
This is the first stage when Alzheimer’s disease is typically diagnosed.
Stage 4: Moderate Decline
In stage four of Alzheimer’s disease, symptoms of Alzheimer’s disease are clearly evident. Patients with stage four Alzheimer’s disease:
- Have difficulty with simple arithmetic
- May forget details about their life histories
- Have poor short-term memory (for example, they may not recall what they ate for breakfast)
- Inability to manage finance and pay bills
Stage 5: Moderately Severe Decline
- During the fifth stage of Alzheimer’s, patients start needing help with day to day tasks. People in stage five of the disease may experience:
- Significant confusion
- Inability to recall simple details about themselves such as their own phone number
- Difficulty dressing appropriately
On the other hand, these patients can maintain many basic functions and still have deeply ingrained memories. They typically can still bathe and use the toilet independently. They also usually still know their family members and some detail about their personal histories, especially their childhood and youth.
Stage 6: Severe Decline
Patients in the sixth stage of Alzheimer’s disease need constant supervision and frequently require professional care. Symptoms include:
- Confusion or unawareness of environment and surroundings
- Major personality changes and potential behavior problems
- The need for assistance with activities of daily living such as toileting and bathing
- Inability to recognize faces except closest friends and relatives
- Inability to remember most details of personal history
- Loss of bowel and bladder control
Stages 7: Very Severe Decline
Stage seven is the final stage of Alzheimer’s disease. Because Alzheimer’s disease is considered a terminal illness, patients in stage seven are nearing death. At this stage, patients lose the ability to respond to their environment and communicate. While they may still be able to utter words and phrases, they have no insight into their condition and need assistance with all activities of daily living.
The Causes of Alzheimer’s
Just as there is currently no true cure, the exact cause of Alzheimer’s disease is still not known. However, we are getting closer.
It is generally agreed upon that age, not genetics as some may believe, is the most significant risk factor. This is due to the fact that Alzheimer’s disease increases exponentially with age in people aged 65 or older.
Other known factors that contribute to Alzheimer’s are genetic variations in apolipoprotein E (ApoE), degeneration of brain cells, mitochondrial dysfunction (brain cells can’t produce energy efficiently), immune system dysfunction, and infectious agents and other environmental factors such as exposure to aluminum, repeated head injury, and malnutrition.
Each one of these factors can contribute to a build-up of beta-amyloid plaque and neurofibrillary tangles in the brain, which results in a chronic inflammatory response, an increase in oxidative stress, and mitochondrial dysfunction. The combination of inflammation, oxidative stress, and mitochondrial dysfunction lead to more amyloid plaque and neurofibrillary tangle build-up, and the vicious cycle continues, progressing the patient to more and more severe stages of Alzheimer’s disease.
One of the causes of this vicious cycle is the decline in glucose metabolism that occurs as we age. In other words, the brain’s ability to use sugar for fuel decreases as it gets older. Not only does this cause lapses in brain function, but it also leads to more oxidative stress and inflammation that results in more beta-amyloid plaque and neurofibrillary tangles. (and the vicious cycle continues.)
A similar problem occurs when people with brain disorders are fed a high carbohydrate diet. In fact, studies have found that just one carbohydrate meal can rapidly reverse the antiseizure effect of the ketogenic diet. A similar phenomenon has been found to occur in Alzheimer’s patients, who tend to experience a worsening in cognitive performance and behavioral issues while they are on a high-carbohydrate diet.
The adverse effects that high-carb diets have on brain health are thought to be caused by sugar. Recent research has shown that blood sugar glucose and Alzheimer’s disease are linked. As blood sugar levels increase, so does the progression of Alzheimer’s disease.
Insulin resistance (the inability of the cells to respond to insulin that typically occurs in type 2 diabetics) has also been found to be correlated with Alzheimer’s disease progression. Some researchers have even referred to Alzheimer’s as “type 3 diabetes” because it may be a late-stage of type 2 diabetes.
Key Takeaway: Alzheimer’s disease is caused by a multitude of known and unknown factors, most of which contribute to the tangling of neurofibrillary proteins and the building up of beta-amyloid plaques. As tangles and plaques accumulate, brain function declines significantly, leading to more plaque and tangle build-up. One of the most studied factors that contribute to Alzheimer’s is the adverse effects that high carbohydrate diets, high blood sugar levels, and insulin resistance have on the aging brain. These negative effects are only exacerbated further if the patient is a carrier of a specific genetic variant of a gene called ApoE.
How Genetics Apply To Alzheimer’s
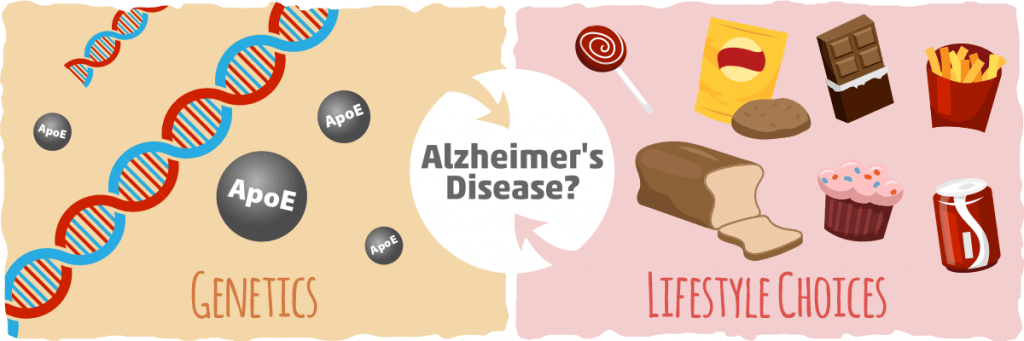
With the popularity of genetic testing on the rise, you may be wondering how genetics play into Alzheimer’s disease risk. The bittersweet reality is that these tests can pick up one gene variant called ApoE, which is intimately connected with Alzheimer’s disease.
More specifically, individuals carrying the ε4 allele are at increased risk of Alzheimer’s Disease compared with those who have the more common ε3 allele, whereas the ε2 allele decreases risk.
Earlier we discussed the factors and theoretical causes of Alzheimer’s disease and these apply to ApoE e4 allele carriers as well. In fact, the only difference between ApoE carriers and non-ApoE carriers is that ApoE carriers are more susceptible to Alzheimer’s disease, and once they do have the disease, it progresses more rapidly. However, if you have the ApoE ε4 allele, it doesn’t mean that you are destined to have issues with Alzheimer’s.
Research studies done on different groups of people throughout the world with the ApoE ε4 allele found that they only had health issues like obesity, diabetes, and Alzheimer’s Disease when they converted to a highly processed western diet and sedentary lifestyle. More specifically, studies on the Yoruba people from Nigeria and the Pima people from Mexico that carried the ApoE ε4 allele had no health issues at all while they were living as their ancestors did. However, once they started living in America and adopting a sedentary lifestyle and westernized diet, they developed Alzheimer’s disease and other health issues.
These findings show us that our genetic variants do not determine our fate, we do. It is clear from these cross-cultural studies that the ApoE ε4 allele is not what we should be focused on when it comes to Alzheimer’s disease; we should be focused on making the right lifestyle and dietary choices.
Key Takeaway: Genetics matter, especially when it comes to Alzheimer’s Disease. If you carry the ε4 allele of the ApoE gene, then you are at a greater risk for Alzheimer’s disease, and if you have it, it will progress more quickly. Fortunately, whether you have the variant or not, there are many ways to improve brain health and prevent or reduce the severity of Alzheimer’s disease.
How The Ketogenic Diet Affects People with Alzheimer’s Disease
After learning that one of the causes of Alzheimer’s disease progression is the issue that many elderly have with glucose metabolism, it is tempting to assume that restricting carbs is the way to go. But before we break into every nursing home and replace bread with bacon, we need to look at some high-quality studies for us to assess the merit of using a ketogenic diet to treat Alzheimer’s disease.
First, let’s look at where most of the research has been done regarding ketogenic diets and Alzheimer’s — in mice.
One group of researchers sought out to find answers by comparing a standard diet to a high-fat, low-carb diet in mice with Alzheimer’s disease. After the study, the authors found that the brains of the mice that were fed a high-fat, low-carb diet had lower levels of beta-amyloid plaque compared to the standard diet fed mice. This suggests that a ketogenic diet may have the ability to reverse plaque accumulation in Alzheimer’s patients.
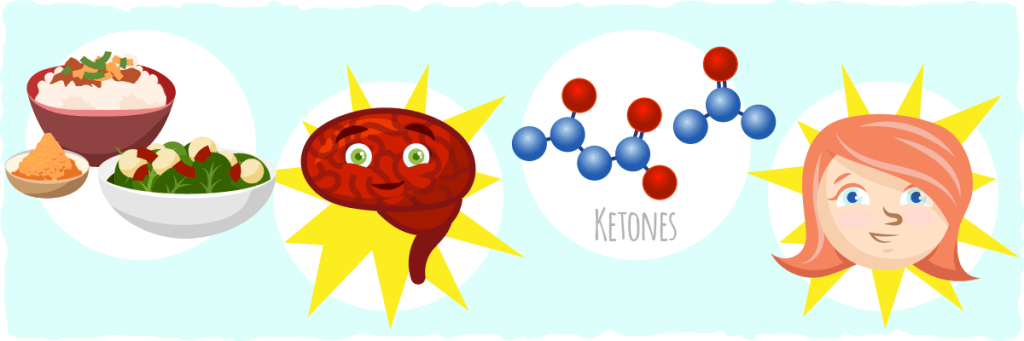
A more recent study helped to clarify why there was a difference between a standard diet and a high-fat, low-carb diet. This study tested the effects that ketones, the bodies alternative fuel source during carb restriction, had in mice with Alzheimer’s disease and in human neuron cells treated with beta-amyloid plaque. The results were pretty astonishing.
Ketones were found to reverse the adverse effects that the beta-amyloid plaque causes, confirming the findings of the earlier study of mice.
One of the ways that the ketones did this was by reducing beta-amyloid levels and keeping the existing beta-amyloid plaques from creating more damage. They also helped restore normal synaptic function and memory performance, which were both originally impaired by the plaque.
However, these findings are only directly applicable to mice — what about the effects that the ketogenic diet has on humans with Alzheimer’s disease?
In one study, twenty-three older adults with mild cognitive impairment were randomly assigned to either a high carbohydrate or very low carbohydrate diet. Following the 6-week dietary intervention period, improved verbal memory performance was observed in participants who ate the low carbohydrate diet.
So, what was the reason for the difference between the diets? Researchers found that insulin levels had a relatively weak correlation with memory improvement. There was one factor, however, that correlated so strongly with the positive effects that researchers believe it is the primary cause of the cognitive benefits of the low carb diet. What was that factor? Ketones.
The researchers found that ketone levels had a strong positive correlation with memory performance. In other words, as ketones levels went up, so did cognitive improvements. These findings indicate that a very low carbohydrate diet like the ketogenic diet can improve cognitive function in older adults who are in the early stages of Alzheimer’s disease.
The only problem is that we have yet to discover a reliable diagnostic tool that can pick up the disease before symptoms emerge. Because of this, it is currently unclear whether or not cognitive decline can always be prevented by the ketogenic diet, but research seems to indicate that it can.
Key Takeaway: The ketogenic diet can help reverse many of the issues that are caused by Alzheimer’s disease. However, there is not enough human clinical trial evidence to establish if the diet can actually reverse or delay the disease. The most conclusive evidence so far can be found from studies that used supplemental ketones in Alzheimer’s patients.
The Powerful Effects of Ketones on Alzheimer’s Patients
Most of the research regarding Alzheimer’s disease and ketones in humans has been conducted with ketone supplements rather than the ketogenic diet. However, they still can provide us with evidence of the effectiveness of both ketone supplements and the ketogenic diet.
Experiments on direct ketone supplementation in humans have shown that the ketone body, β-hydroxybutyrate, improved cognitive function of Alzheimer’s patients. Even at lower doses, ketone supplementation has been shown to have a positive effect. For example, one study found that, just by providing the body with a minimal dose of ketone bodies, it was able to supply a fraction of the energy that the brain needed and improve cellular function. In short, giving your body a dose of ketones, small or large, can help preserve the function of aging brain cells that are struggling with metabolizing glucose.
Many other clinical trials have validated the neurological benefits that ketones have by giving MCT oil (a fat found in coconut oil that is converted into ketones in the liver) to Alzheimer’s patients and testing their memory. They found that patients in the earlier stages of the disease experienced greater memory recall and cognitive function that directly correlated with their ketone levels. However, little to no effect was found for Alzheimer’s patients with the APOE ε4 allele when they were given MCTs.
Promising Results for A Severe Case of Alzheimer’s Disease
Although It’s true that many trials on ketone supplementation found that they have little to no effect on Alzheimer’s patients with the APOE ε4 allele, there’s still hope.
In a recent case study, A 63 year-old man with the APOE ε4 allele AND advanced Alzheimer’s Disease supplemented his regular diet with coconut oil and medium chain triglycerides to increase his ketone levels. After just over two months, his score on the Mini Mental State Exam, a test of global cognitive function, increased from an extremely low 12 to 20 (out of a max 30).
After two years of this protocol, his cognitive ability and daily living functions both improved. What’s even more surprising is that his MRI showed no further brain atrophy!
To get even better results, the patient added a ketone ester supplement to his dietary regimen, and it provided even further improvements in his mood, quality of life, and memory.
As a result, the authors of the case study concluded that ketosis does appear to be highly beneficial for ApoE4 carriers, even if prior studies indicate it’s even more helpful for those without this risk factor.
Key Takeaway: Although many studies indicate that ketone supplementation only helps mild to moderate cases of Alzheimer’s disease without the ApoE ε4 allele, this case study suggests otherwise. More specifically, medium chain triglycerides, coconut oil, and ketone esters have the potential to help people who have advanced Alzheimer’s disease AND the ApoE ε4 allele.
How Ketones and the Ketogenic Diet Work to Fight Alzheimer’s Disease
Now that we know what happens when we increase ketone levels and cut out carbs, let’s figure out how this happens.
Although a couple of suggestions are riddled throughout this article, here is a list of the effects that the ketones have on Alzheimer’s patients:
- Decrease oxidative damage. Oxidative damage is one of the factors that cause plaque and tangle build up in the brain. Ketones generate much lower levels of oxidative stress in the brain compared to sugar.
- Provide neuroprotective properties. Ketones have antioxidant effects that help protect neurons and other brain cells from damage.
- Increase mitochondrial production. As we age, our mitochondria tend to get sluggish and have more problems, especially in the brain. One way to counteract these effects is by burning ketones. Ketones trigger the production of new mitochondria and the improvement of mitochondrial pathways in older mitochondria.
- Regulate the glutamatergic neurotransmitter system. The glutamatergic system in the brain is essential for learning and memory, but when it is consistently activated, it causes neurodegeneration, which progresses Alzheimer’s disease even further. When the body uses ketones for fuel, GABA levels tend to increase significantly. Why does this matter? Well, GABA is a neurotransmitter that helps keep the glutamatergic system from becoming too active and destroying the brain.
- Promote the expression of brain-derived neurotrophic factor (BDNF). BDNF is a protein that enhances the growth, maturation (differentiation), and maintenance of brain cells. Ketones have been found to trigger the expression of BDNF indirectly.
Keep in mind that these four effects only cover what ketones do to the brain. The ketogenic diet confers some extra benefits, including:
- Decreased blood sugar levels. The ketogenic diet lowers blood sugar levels significantly for the duration of the diet. This decreases the amount of glucose that the brain uses, reducing the problems that can be caused by glucose metabolism that we discussed earlier.
- Reduced insulin levels. The more we spike our insulin levels, the more our brain will become resistant to insulin. As our cells become resistant to insulin, they struggle to get the energy that they need and begin to malfunction. By reducing insulin levels with the ketogenic diet, you can make your cells more sensitive to insulin, while you provide them with an alternative energy source at the same time.
- Autophagy activation. As a result of carbohydrate restriction, a cellular cleaning process called autophagy is activated. This process is essential for maintaining healthy cells and can help improve brain cell function as well.
These aren’t all the benefits of the ketogenic diet, but they are most relevant for Alzheimer’s patients.
Altogether, the ketogenic diet and ketones address many of the factors that cause Alzheimer’s disease, which explains why many clinical trials and animal studies have found such promising results.
The Ketogenic Diet vs. Ketone Supplements — Which One is Better?
Although most of the research has been on ketone supplements, this does not mean that the ketogenic diet is inferior to these supplements. In fact, the opposite is true. Not only does the ketogenic diet increase ketone levels, but it reduces insulin and glucose levels as well. By lowering insulin and glucose levels and increasing ketones at the same time, the ketogenic diet gives the brain the fuel it needs while eliminating two of the factors that can cause plaque and tangle build up. Ketones supplements cannot do all of this for you.
Either way, you or your loved ones can get results from both options. What you choose depends on what you are willing to commit to and what is pertinent to your needs and your lifestyle. If ketone supplements are easiest for you, try them out. But if they aren’t working as well as you’d like, then the ketogenic diet is the best option for you.
Can Keto Cure Alzheimer’s?
No supplement or diet has been found to cure Alzheimer’s disease. At this point, the research suggests that the best strategy is to diagnose the disease as quickly as possible and take steps to prevent its progression. In other words, the best cure for Alzheimer’s disease is prevention.
However, this doesn’t mean that we won’t find a cure in the future. Just as we’ve learned in recent years that conditions like type 2 diabetes can be reversed with diet, there is promise for the potential to reverse Alzheimer’s Disease as well.
In fact, we might find in the future that this horrible disease can be healed with a complete shift in diet and lifestyle. We already know the ketogenic diet may be the best dietary choice for Alzheimer’s patients, but what about other lifestyle choices?
Other Ways to Protect Your Brain and Potentially Reverse Alzheimer’s Disease
Besides a ketogenic diet and ketone supplements, there are plenty of other ways to improve brain health, including:
- Eat low-glycemic, whole foods. Remove the sugars, carbs, processed foods, alcohol, and inflammatory omega-6 rich processed oils as they all contribute to brain aging. Replace them with wholesome fats like low-carb nuts, avocados, grass-fed meats, and high-quality oils.
- Eat more cruciferous vegetables. Cruciferous vegetables contain sulforaphane, a compound that activates a transcription factor called Nrf2.What this means is that sulforaphane helps to set off a cascade of processes that detoxify and protect the brain from oxidative damage.
- Supplement with omega-3-rich fats. Eat wild fatty fish or take high-quality fish oil supplements daily to reduce inflammation. 1 to 3 grams of EPA + DHA per day is typically recommended for most people.
- Drink coffee or tea. Habitual caffeine intake may protect against cognitive impairment. In studies done on mice, caffeine has been found to suppress the buildup of beta-amyloid plaque in the brain.
- Try curcumin. Like caffeine, circumin can prevent plaque build up, and it has the added ability to remove plaque as well. It is also known to lower cholesterol, reduce oxidative damage, and remove metals that accumulate in the brain like iron and copper. The most effetive way to get these benefits is by taking one of these variations of curcumin: curcumin with black pepper (piperine), curcumin phytosomes complexed with phosphatidylcholine (Meriva or BCM-95), Curcumin nanoparticles (THERACURMIN), or Water-soluble curcumin (polyvinyl pyrrolidone).
- Take B vitamins. B vitamins are essential for brain health. More specifically, vitamins B3 and B1 can improve cognition and prevent plaque build-up.
- Move more. Physical activity has been shown to slow down or prevent brain diseases and continuing cognitive decline.
- Sleep for at least eight hours a night. Chronic lack of quality sleep has been linked to cognitive dysfunction among other problems.
- Practice stress relief. Chronic stress is another thing that is harmful to your brain, negatively impacting insulin sensitivity and memory. Incorporating calming practices like yoga, meditation, and deep breathing into your life is the best way to reduce anxiety and stress.
- Reach outside of your comfort zone every day. When the brain feels challenged, such as when you’re trying something new or learning a new skill, it grows new synaptic connections and improves many of its functions. Think of it like lifting weights — by increasing the weight little by little each week (challenging your brain) you stimulate muscle growth (improve brain function).
Putting it All Together
Alzheimer’s disease is still a mystery in many aspects, but we understand some the factors that contribute to it and how to slow it down.
Although we are not entirely sure how to prevent or cure Alzheimer’s disease, we do have clues that give us some hope that it is possible. For example, it is obvious that inactivity and high-carb diets with heavily processed foods contribute to the progression of Alzheimer’s tremendously, while ketones and low-carb diets have potent positive effects on the brains of healthy people and Alzheimer’s patients.
The current evidence suggests that supplementing with ketones and/or following the ketogenic diet is a safe and effective approach for helping people with Alzheimer’s Disease with the potential to stop the disease from progressing entirely. Some animal model evidence even suggests that the disease can be reversed. However, the approach to treating Alzheimer’s should be multifaceted for the best results.
Here are some lifestyle changes one should consider implementing when faced with Alzheimer’s Disease:
- Adopt a low-carb, high-fat ketogenic diet. Consult our beginner’s guide to learn how to follow the diet and what to expect.
- Supplement with ketones by taking MCTs or ketone esters.
- Eat primarily whole foods, especially low-carb cruciferous vegetables.
- Consume plenty of omega-3-rich fats.
- Drink coffee or tea.
- Try supplementing with curcumin and b vitamins.
- Increase physical activity levels.
- Sleep for at least eight hours a night.
- Implement stress relief practices.
- Try something new and learn every day.
By following these simple suggestions, you can help protect your brain and possibly even reverse Alzheimer’s disease.
Sources:
- The neuroprotective properties of calorie restriction, the ketogenic diet, and ketone bodies — Science Direct
- The Ketogenic Diet as a Treatment Paradigm for Diverse Neurological Disorders — NCBI
- Short term improvement of migraine headaches during ketogenic diet: a prospective observational study in a dietician clinical setting — NCBI
- KETONES INHIBIT MITOCHONDRIAL PRODUCTION OF REACTIVE OXYGEN SPECIES PRODUCTION FOLLOWING GLUTAMATE EXCITOTOXICITY BY INCREASING NADH OXIDATION — NCBI
- Effects of beta-hydroxybutyrate on cognition in memory-impaired adults. — NCBI
- The therapeutic implications of ketone bodies: the effects of ketone bodies in pathological conditions: ketosis, ketogenic diet, redox states, insulin resistance, and mitochondrial metabolism. — NCBI
- Insulin Regulates Brain Function, but How Does It Get There? — Diabetes
- Neuroprotective and disease-modifying effects of the ketogenic diet — NCBI
- Alzheimer’s could be caused by excess sugar: new study finds ‘molecular link’ — The Telegraph
- Ketogenic diets and Alzheimer’s disease — Science Direct
- Ketones to combat Alzheimer’s disease — PLOS Neuro Community
- The Ketogenic Diet: Making a Comeback — Ingenta Connect
- Ketogenic Diet in Neuromuscular and Neurodegenerative Diseases — Hindawi
- Effects of ketone bodies in Alzheimer’s disease in relation to neural hypometabolism, β-amyloid toxicity, and astrocyte function — Journal of Neurochemistry
- Stages of the pathologic process in Alzheimer disease: age categories from 1 to 100 years. — NCBI
- Apolipoprotein E and Alzheimer disease: risk, mechanisms, and therapy — NCBI
- Study of the ketogenic agent AC-1202 in mild to moderate Alzheimer’s disease: a randomized, double-blind, placebo-controlled, multicenter trial — Nutrition and Metabolism
- THE NEUROPROTECTIVE PROPERTIES OF CALORIE RESTRICTION, THE KETOGENIC DIET, AND KETONE BODIES — NCBI
- High carbohydrate diets and Alzheimer’s disease. — NCBI
- The apolipoprotein E4 allele is not associated with an abnormal lipid profile in a Native American population following its traditional lifestyle. — NCBI
- Alzheimer’s disease, genes, and environment: the value of international studies. — NCBI
- How to Prevent Alzheimer’s Disease — Dr. John Day
- Ketones block amyloid entry and improve cognition in an Alzheimer’s model — Science Direct
- A new way to produce hyperketonemia: use of ketone ester in a case of Alzheimer’s — NCBI
- Alzheimer’s disease, β-amyloid, glutamate, NMDA receptors and memantine – searching for the connections — NCBI
- Your Brain on Ketones — Psychology Today
- BDNF gene — Genetics Home Reference
- Exercise Enhances and Protects Brain Function — Exercise And Sport Sciences Reviews
- Stress- and treatment-induced elevations of cortisol levels associated with impaired declarative memory in healthy adults — Life Sciences
- Cortisol-Induced Insulin Resistance in Man: Impaired Suppression of Glucose Production and Stimulation of Glucose Utilization due to a Postreceptor Defect of Insulin Action — The Journal of Clinical Endocrinology & Metabolism
- What Are the 7 Stages of Alzheimer’s Disease? — Alzheimer’s
- Exercise promotes the expression of brain derived neurotrophic factor (BDNF) through the action of the ketone body b- hydroxybutyrate — eLife Sciences
- The Nrf2/ARE Pathway as a Potential Therapeutic Target in Neurodegenerative Disease — NCBI
- Caffeine suppresses β-amyloid levels in plasma and brain of Alzheimer’s transgenic mice — NCBI
- The effect of curcumin (turmeric) on Alzheimer’s disease: An overview — NCBI
- Vitamin B1 (thiamine) and dementia. — NCBI
- Vitamin B3 reduces Alzheimer’s symptoms, lesions — UCI News
- Curcumin — Examine