According to the World Health Organization, cardiovascular disease (which is also commonly referred to as heart disease) is the leading cause of death globally.
On the surface, this sounds like a dreadful omen for humanity, but there is some sweetness to this bitter news once we realize that heart disease is preventable and, in some cases, reversible.
What is Heart Disease?
Heart diseases are a group of disorders of the heart and blood vessels. In general, they fall into these categories:
- Coronary heart disease – disease of the blood vessels supplying the heart muscle.
- Cerebrovascular disease – disease of the blood vessels supplying the brain.
- Peripheral arterial disease – disease of blood vessels supplying the arms and legs.
- Rheumatic heart disease – damage to the heart muscle and heart valves from rheumatic fever, caused by streptococcal bacteria.
- Congenital heart disease – malformations of heart structure existing at birth.
- Deep vein thrombosis and pulmonary embolism – blood clots in the leg veins, which can dislodge and move to the heart and lungs.
The most common, preventable, and reversible type of heart disease is coronary heart disease or coronary artery disease. This occurs when the arteries that supply blood to heart muscle become hardened and narrowed as plaque accumulates on their inner walls. The technical term for this is atherosclerosis.
As atherosclerosis worsens, less blood is allowed to flow through the arteries. As a result, the heart muscle can’t get the blood or oxygen it needs. This can lead to chest pain (angina) or a heart attack.
Most heart attacks happen when a blood clot suddenly cuts off the heart’s blood supply, causing permanent heart damage. These clots typically form at the site of a ruptured arterial plaque.
Over time, atherosclerosis can also weaken the heart muscle and contribute to heart failure and changes in normal heartbeat rhythm.
Simply put, coronary heart disease is an insidious process that impairs cardiovascular function and sets the stage for traumatic events, such as heart attacks and strokes. When we frame the condition in this way, however, it may seem like there isn’t much you can do to prevent or reverse it.
In reality, the opposite is true. Diet and lifestyle play a crucial role in preventing further plaque build-up, with the potential to help us reduce atherosclerosis as well.
How is Heart Disease Preventable and Reversible?
Although there are many genetic factors that determine your risk of heart disease, it is still preventable and can be reversible. This is because the most common cause of heart disease – atherosclerosis – is created by modifiable factors (i.e., elements that are under our control).
However, don’t let the fact that atherosclerosis is the buildup of fatty plaques in your arteries fool you. This doesn’t mean that fat clogs your arteries. In fact, fat isn’t the problem.
Interestingly enough, atherosclerosis isn’t even the problem – It is the solution to the immediate problem that is caused by oxidized LDL cholesterol.
LDL – The Misunderstood Lipoprotein and Plaque Formation
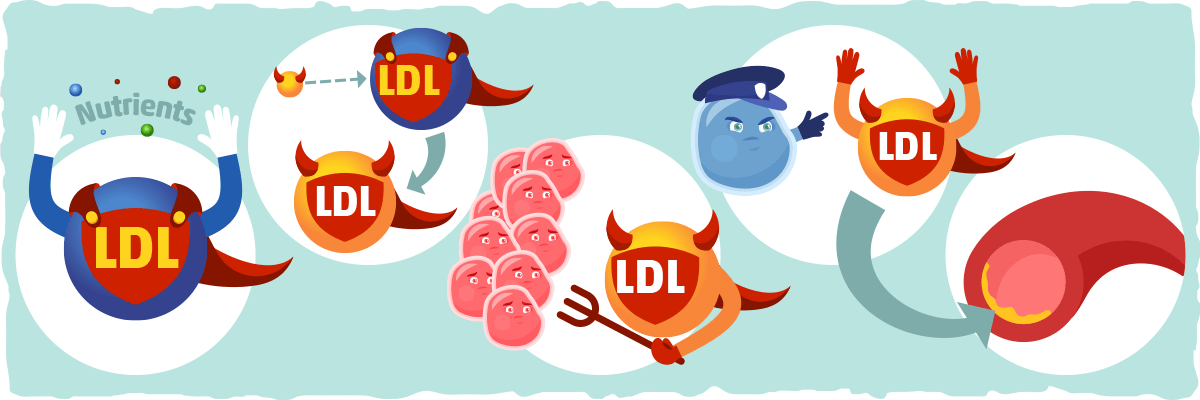
LDL (low-density lipoprotein) is commonly referred to as “bad cholesterol”, but it is actually critical for our survival.
You can think of LDL as a superhero with a very short temper. LDL brings essential nutrients, such as cholesterol and vitamins, to our cells. Unfortunately, if the LDL interacts with free radicals and volatile molecules in the blood, it begins to oxidize.
The now oxidized LDL goes on a temper tantrum causing damage to the endothelial cells (cells that line the inside of our blood vessels). The endothelial damage triggers macrophages (immune system cells) to neutralize the oxidized LDL and prevent further destruction.
The macrophage convinces the oxidized LDL to hand in its superhero costume and become an inert, non-toxic fatty plaque that resides between the walls of the blood vessel.
Our body creates this plaque to keep the oxidized LDL from damaging more cells, which is why atherosclerosis is part of the (short-term) solution. The direct pay-off being that the oxidized LDL can no longer harm healthy cells.
In the long-term, however, this shortsighted solution turns into a bad omen, increasing our risk of heart disease, heart attack, and stroke if we don’t make the appropriate changes to our diet and lifestyle.
LDL’s involvement in this plaque building process is the primary reason why it has become such a demonized particle. However, so many factors play a role in increasing the likelihood of heart disease that simply reducing LDL numbers is not enough. This is evidenced by the fact that the disease often develops in the presence of lower LDL levels as well.
Focusing solely on LDL to assess heart disease risk is like blaming the water when your sink drain gets clogged. You can keep the sink from backing up by reducing the flow of water through the drain, but doing so does not address the other issues contributing to the “clog.”
Risk Factors for Heart Disease
To better assess cardiovascular disease risk, we must take notice of these key risk factors that contribute to atherosclerosis:
- Age. Aging, directly and indirectly, contributes to the development of atherosclerosis and heart disease
- Sex. Men generally have a higher risk of heart disease. However, women’s risk increases after menopause.
- Family history. A family history of heart disease increases your risk of coronary artery disease, especially if one of your parents developed it at an early age.
- Nicotine constricts blood vessels while the toxins in the smoke damage their inner lining, increasing the likelihood of developing atherosclerosis. Heart attacks are more common in smokers than in nonsmokers.
- Poor diet. Diets that are high in saturated fat, salt, sugar, and cholesterol can contribute to the development of heart disease. Low fruit and vegetable intake can also increase risk.
- High blood pressure. Uncontrolled high blood pressure can result in hardening and thickening of your arteries. This is also can provoke heart attacks and strokes.
- Abnormal blood lipids. High triglycerides and high levels of specific LDL particles greatly increase the risk of atherosclerosis formation.
- Type 2 diabetes. Diabetes increases the risk of heart disease directly by sustaining a plaque-promoting internal environment and indirectly by worsening the other risk factors.
- Excess body fat. Carrying excess body fat typically worsens other risk factors and increases inflammation levels.
- Physical inactivity. Lack of exercise is associated with many forms of heart disease and some of its other risk factors.
- Stress and other psychosocial factors. Unrelieved stress may damage arteries, cause heart issues, and worsen other risk factors for heart disease.
Of eleven these risk factors, studies indicate that we have the most control the ones that have the biggest impact on heart disease. One observational study of 52 countries, for example, found that eight modifiable risk factors – i.e., abnormal blood lipids, smoking, high blood pressure, diabetes, abdominal obesity, psychosocial factors, consumption of fruits, vegetables, and alcohol, and regular physical activity – accounted for most of the heart attack risk worldwide in both sexes and at all ages in every inhabited continent.
This is a noteworthy finding because it shows that one of the most life-threatening complications of atherosclerosis, heart attack, is associated with the same modifiable risk factors across the globe.
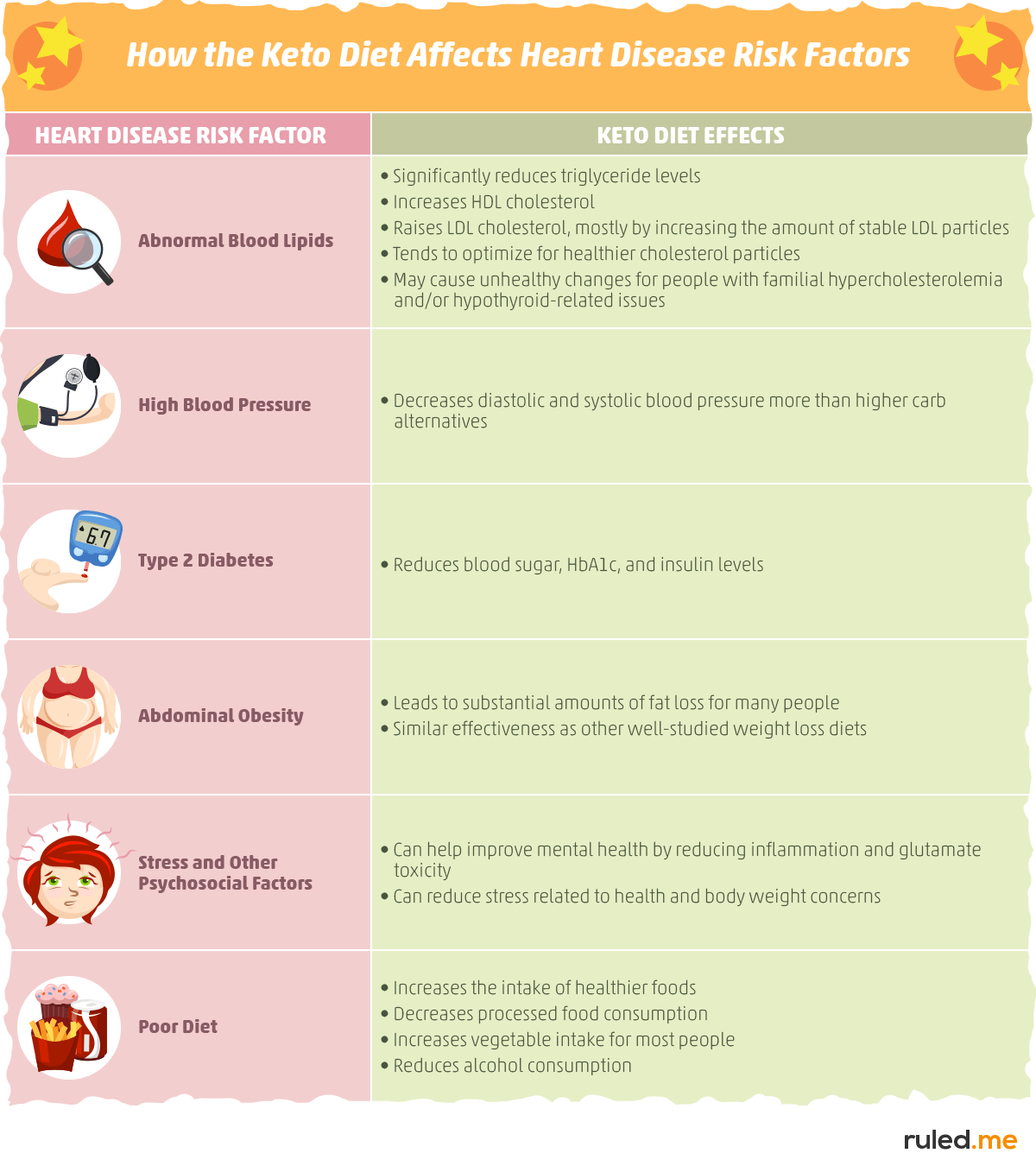
Furthermore, six of these eight risk factors identified in the study – i.e., abnormal blood lipids, high blood pressure, type 2 diabetes, abdominal obesity, some psychosocial factors, and consumption of fruits, vegetables, and alcohol – can all be addressed by following the right diet. The keto diet, for example, has been found to improve all six. below, you can reference the graphic for a summarized version:
The Ketogenic Diet & Heart Disease: How Does Keto Impact These Risk Factors?
Because of its focus on fat consumption, the keto diet is concerning to many doctors, dieticians, and health advocates. However, the truth as to what happens when we eat more fat and cut the carbs is much more complex.
Put simply, several studies indicate that the keto diet can help most people reduce their heart disease risk while small subsets of the population may significantly increase their risk by following a standard keto diet.
To help us decipher between the two and develop a deeper understanding of what keto can do for heart disease, let’s take a look at how keto affects the six risk factors that can be addressed with diet.
Here’s a clickable table of contents for what we will cover:
- Keto, Cholesterol, and Triglycerides
- How the Keto Diet Affects Blood Pressure Levels
- Keto, Insulin Resistance, and Type 2 Diabetes
- Keto for Fat Loss
- The Impact of Keto on Wellbeing, Stress, and Depression
- How Keto Changes Your Plant and Alcohol Intake for Better Health
- Can Keto Cause Heart Problems?
- Keto vs. the Mediterranean Diet for Heart Disease
- What Would The Best Diet for Heart Disease Look Like?
- The Mediterranean Ketogenic Diet
- What is the Best Diet for Heart Disease?
- Practical Applications for Your Diet
Keto & Abnormal Blood Lipids: The Impact on Triglycerides and Cholesterol Levels
The most widely studied lipids are low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides. There are other lipid particles that could give us a more complete picture, but the data on them is too scarce at this point.
Keto and Cholesterol: A Cause of Concern?
Out of all the risk factors for heart disease, the effects that keto has on cholesterol levels attracts the most controversy.
Many doctors, dieticians, and diet researchers will immediately reject any diet that advocates for more fat consumption. To them, the potential for harm is obvious.
More fat means more saturated fat which typically leads to higher LDL cholesterol levels and an increased risk for heart disease. Since the keto diet is one of the most popular high-fat diets, the connection between keto and heart disease is one of the most publicized risks of the diet.
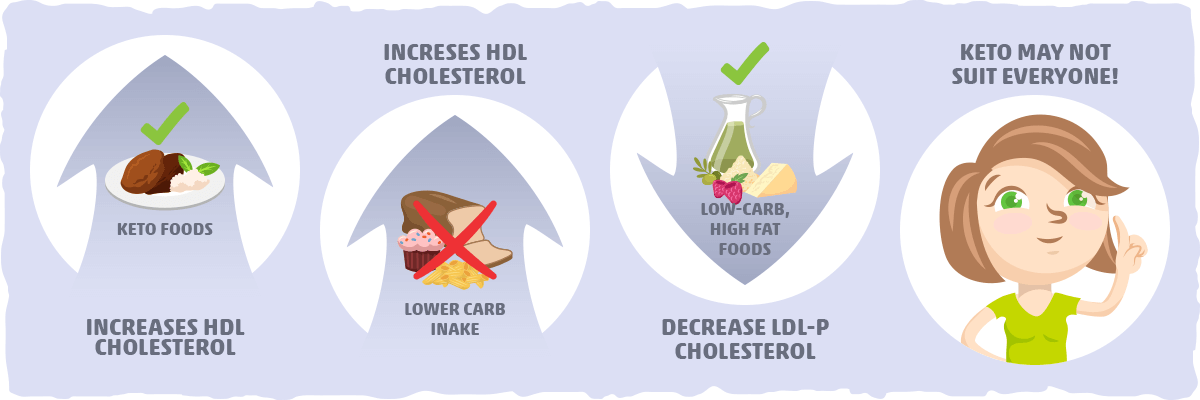
On the other end of the spectrum, low-carb doctors, dieticians, and researchers argue that the rise in cholesterol caused by keto represents an optimization of cholesterol levels. This is based on an abundance of low-carb and keto diet research that has shown:
- Ketogenic diets increase the concentrations of heart-healthy HDL cholesterol more than low-fat, high-carb diets.
- Lowering carbohydrate consumption in healthy individuals also leads to higher levels of HDL cholesterol.
- Low-carb, high-fat diets decrease LDL particle concentration (LDL-P) and increase the size of LDL cholesterol. Since LDL-P is more strongly associated with heart disease risk than LDL-C, this gives the argument for cholesterol level optimization more credibility.
- Ketogenic diets decrease the amount of harmful VLDL cholesterol in the blood.
- The increase in LDL cholesterol that commonly occurs with keto dieting appears to be limited to large LDL, which much more stable and less atherogenic than other LDL particles.
All in all, this is strong evidence that shows the carbohydrate restriction as emphasized in the ketogenic diet can be a heart-healthy choice.
However, this doesn’t mean that the “keto is bad for the heart” side of the argument is entirely wrong. A small subset of the population may not fare well, from a heart health perspective, when they eat a high-fat, low-carb diet.
More specifically, A high-fat, low-carb diet may not be a healthy option for people with one or more of the following conditions:
- Familial hypercholesterolemia
- Hypothyroid-related issues
- Chronic inflammation and stress that aren’t responding well to the keto diet
The simplest, most accessible way to figure out if the keto diet may not be ideal for you is if your total-to-HDL cholesterol ratio is above 4 and/or your LDL-P (not your LDL-C) remain high or increase after starting the keto diet. If this is the case for you, then it may indicate that your particular condition requires you to make adjustments to your keto diet (i.e., following a Mediterranean keto diet as we’ll learn about later) or to follow a different dietary approach altogether.
To take a closer look at the keto diet and cholesterol research and what this means for you, check out our keto and cholesterol article.
Keto vs. Triglyceride Levels
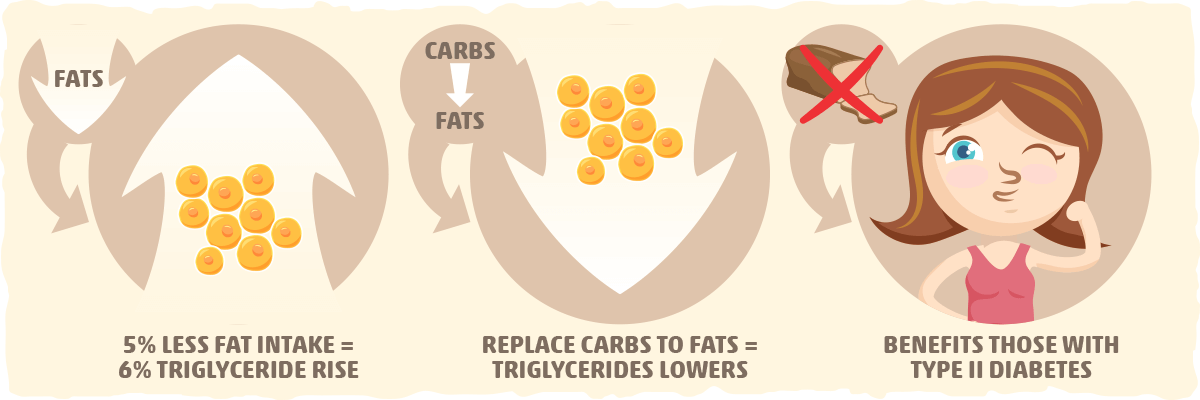
In contrast to cholesterol, there is much less controversy surrounding how diet impacts triglyceride levels. In fact, meta-analyses show a strong relationship between carb consumption and blood triglycerides: With every 5% decrease in total fat intake, triglyceride levels are predicted to increase by 6%.
Furthermore, researchers also discovered that with every 1% isoenergetic (same calorie content) replacement of carbohydrate with each category of fatty acid (saturated, monounsaturated, and polyunsaturated), there was a predictable decrease in triglyceride levels. The most significant decrease was found with polyunsaturated fat (which is a major part of the Mediterranean diet).
It also didn’t matter if the carbohydrate was from table sugar or whole food. Replacing any carbs with the same calorie content from fat led to a decrease in triglyceride levels. Plus, these results may be even better for people with type 2 diabetes — a condition that can also be improved by reducing carbohydrate consumption.
For a closer look at the research on triglycerides and what it means for you, check out our article on triglyceride-lowering diets.
Key Takeaways – The Keto Diet Vs. Blood Lipids
The current literature indicates that keto typically has these effects on blood lipids:
- Increases HDL cholesterol levels.
- Increases LDL cholesterol levels, primarily by increasing LDL particle size. This may be optimal because larger LDL particles are much less atherogenic than smaller varieties.
- Decreases triglyceride levels.
In general, there is plenty of high-quality data supporting that the keto diet can improve blood lipids for most people.
However, there are a few subsets of the population may experience a worsening of blood lipid levels after following a high fat, low carb diet. This is why it is crucial to monitor your health when making any major dietary change.
For an in-depth breakdown of the research and practical strategies for optimizing your blood lipids, please read through these articles:
Is the Keto Diet Good for Your Blood Pressure?
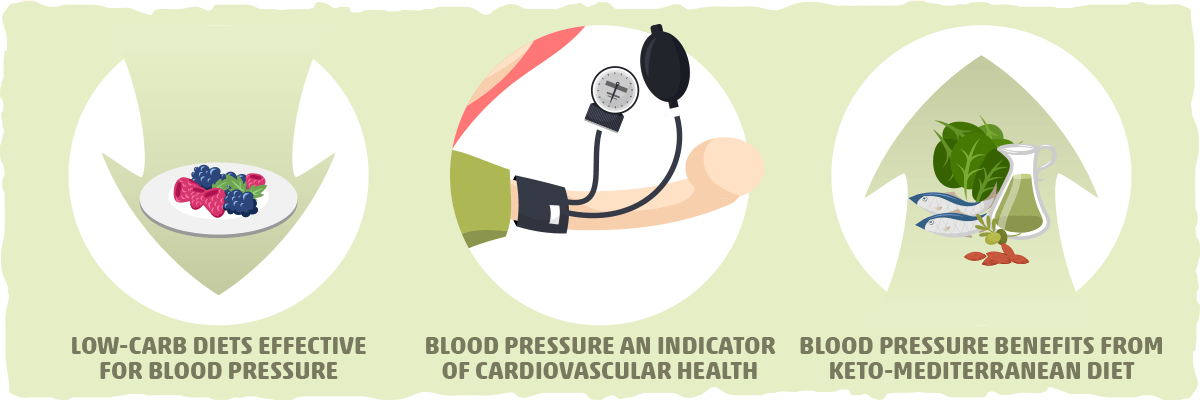
Research shows that blood pressure is a crucial indicator of your risk of developing cardiovascular diseases. If left untreated, high blood pressure can really take a toll on your heart and vascular health and make serious complications more prevalent.
Fortunately, diet can be used as an effective tool for reducing blood pressure. Evidence shows that keto may be one of the best approaches for managing high blood pressure. More specifically:
- Studies indicate that low-carb diets are more effective than both higher-carbohydrate diets and a low-fat diet coupled with weight loss medication that also lowers blood pressure.
- One study found that a ketogenic Mediterranean diet high in healthy fats, fish, and vegetables may have an even more substantial impact of blood pressure levels. The blood pressure reduction achieved with this dietary approach was similar to the results achieved in trials on the DASH diet (which is a diet specifically designed to help treat and prevent high blood pressure).
If you’d like to learn more about blood pressure and the keto diet, check out our article titled “Can a Low Carb Diet Lower Blood Pressure?”
The Ketogenic Diet, Insulin Resistance, and Type 2 Diabetes
In general, the risk of heart disease-related death and stroke are twice as high in people with diabetes. This startling statistic can be traced back to two key issues:
- Type 2 diabetics are typically also struggling with several other risk factors for heart disease.
- High blood sugar levels drive inflammation and slow blood flow, which both can accelerate atherosclerosis.
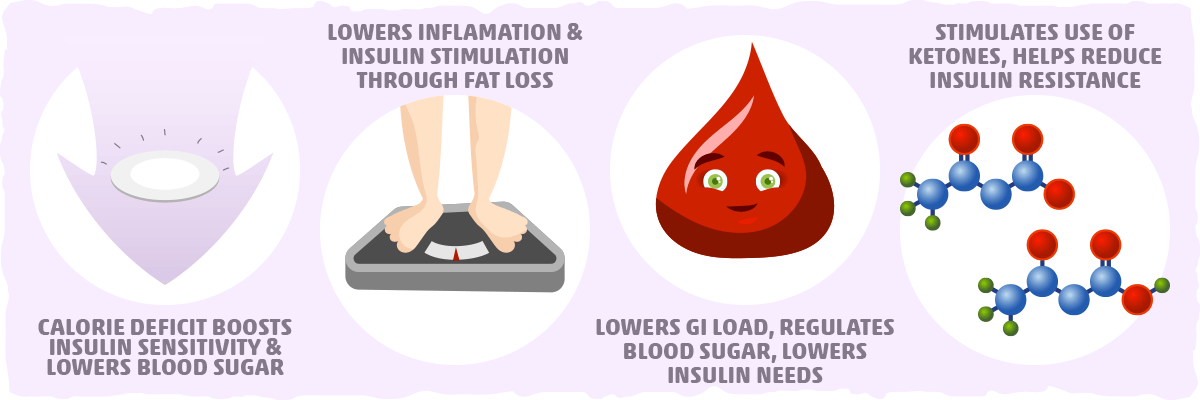
Both of these issues can be addressed with the keto diet. More specifically, when study subjects with type 2 diabetes followed a low-carbohydrate ketogenic diet, they lost substantial amounts of weight, and their blood sugar and HbA1c levels drop significantly. Even studies that put healthy individuals on a ketogenic diet found similar improvements.
In fact, many studies suggest that ketogenic diets are more effective in managing and preventing diabetes when compared to low-calorie diets. Altogether, these promising results can be explained in part by the fact that the keto diet:
- Helps us sustain a calorie deficit, which increases insulin sensitivity and lowers blood sugar and HbA1C.
- Helps us lose fat, which reduces inflammation and the production of signaling molecules that can provoke insulin resistance and heart disease.
- Significantly reduces our glycemic load, which helps us regulate blood sugar levels and decrease our insulin needs.
- Stimulates the use of ketones, which can help reduce insulin resistance and inflammation levels.
If you’d like to take a closer look at the research, check out “The Ketogenic Diet and Diabetes.”
Keto for Fat Loss
One of the primary drivers of chronic inflammation is excess visceral fat (the fat that accumulates around your organs). This type of fat essentially acts as an endocrine gland, secreting different hormones that stimulate inflammatory activities in the body.
By promoting chronic inflammation, visceral fat indirectly creates an internal environment that facilitates atherosclerosis and increased blood pressure. Being overweight is also usually accompanied by insulin resistance and higher blood sugar levels, which will further increase inflammation and heart disease risk.
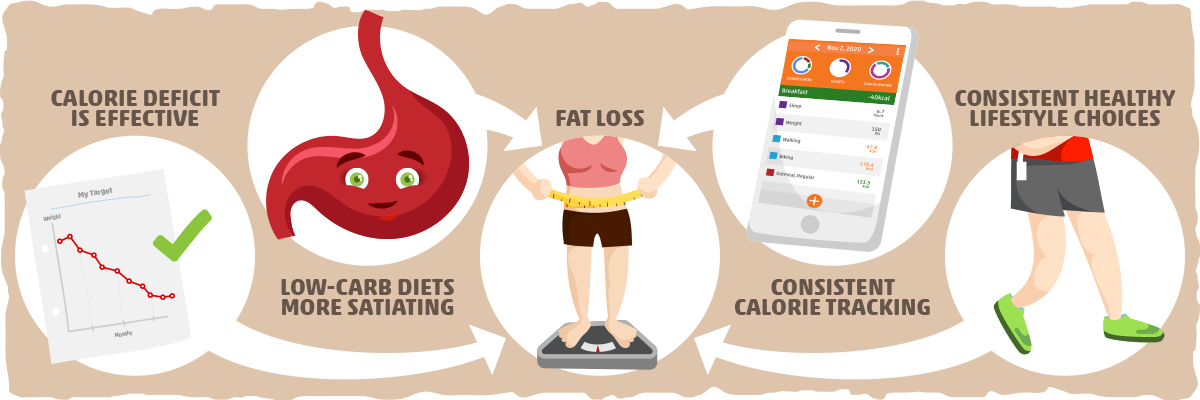
As you may already know, the keto diet is one of the best diets for fat loss. In fact, the bulk of research indicates that the ketogenic diet may be slightly more effective than other common weight loss diets in helping you lose weight and shed body fat.
There is a lot of confusion regarding how keto achieves these results, so here is a brief overview of the research to set the record straight:
- Being in a calorie deficit is the key to weight loss. Low carb diets are effective not because carbs are fattening, but because cutting carbs increases the satiety of the diet and naturally reduces calorie consumption.
- Consistency is important. Most of the studies that yielded good results did so because subjects kept track of their calorie intake and made healthy lifestyle choices that they could sustain for the long-term.
Overall, the keto diet is a one-stop shop for improving many common heart disease risk factors, particularly overweight/obesity. To learn more about losing excess fat with a keto lifestyle, check out these resources:
The Potential Impact that Keto Can Have on Mental Health
Mental health has a significant impact on heart disease risk, directly and indirectly. Directly, through the effects of chronic stress on heart function, and indirectly, by contributing to other risk factors such as high blood pressure, visceral fat accumulation, high blood pressure, high blood sugar levels, and abnormal blood lipid levels.
Although dietary changes may not be the first thing you think of doing when you are trying to improve the psychological aspects of life, diet can have a substantial impact. Take the keto diet for example.
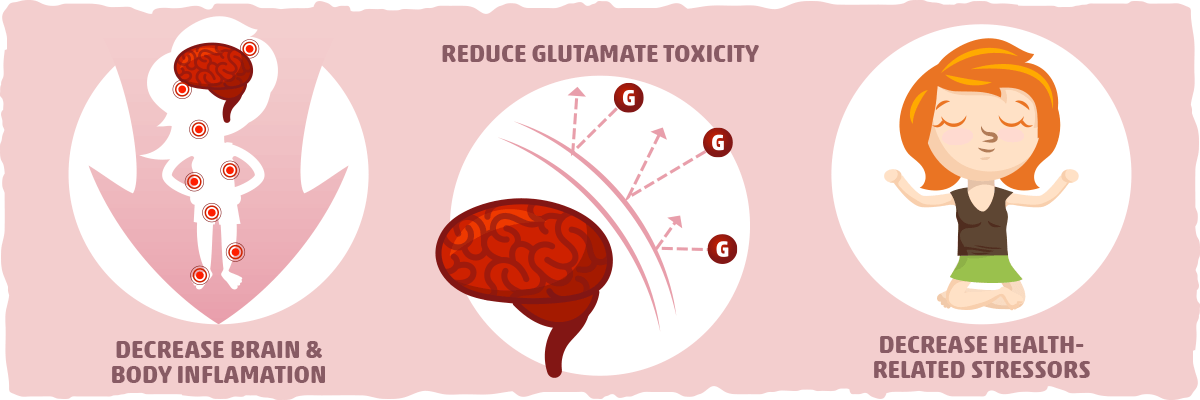
Research indicates that carb restriction may help address mental health on multiple levels:
- By decreasing inflammation throughout the body and brain. Chronic inflammation can lead to poor mental and physical health. Plus, anti-inflammatory practices, such as exercise and consuming omega-3 fatty acids, have been shown to have a strong effect on mental health. Since keto dieting can help reduce inflammation levels, it may have similar effects as well.
- By reducing glutamate toxicity. When there’s too much excitement (caused by the neurotransmitter glutamate) in the brain, that’s known as neurotoxicity. At its worst, neurotoxicity causes seizures as we see in those with epilepsy. Depression and other mood disorders also have links to neurotoxicity. One way to regulate glutamate activity is by decreasing carb intake and increasing ketone use.
- By decreasing health-related stressors. The keto diet provides us with a way to lose weight and improve health at the same time. This can help us feel like we have more control over our health and body composition, resulting in a greater sense of wellbeing.
Although the effects that the keto diet has on mental health have yet to be studied directly, it is reasonable to speculate that this dietary change can have a significant impact on the psychological aspects of our lives as well.
How Keto Improves Your Food and Drink Choices, Lowering Heart Disease Risk
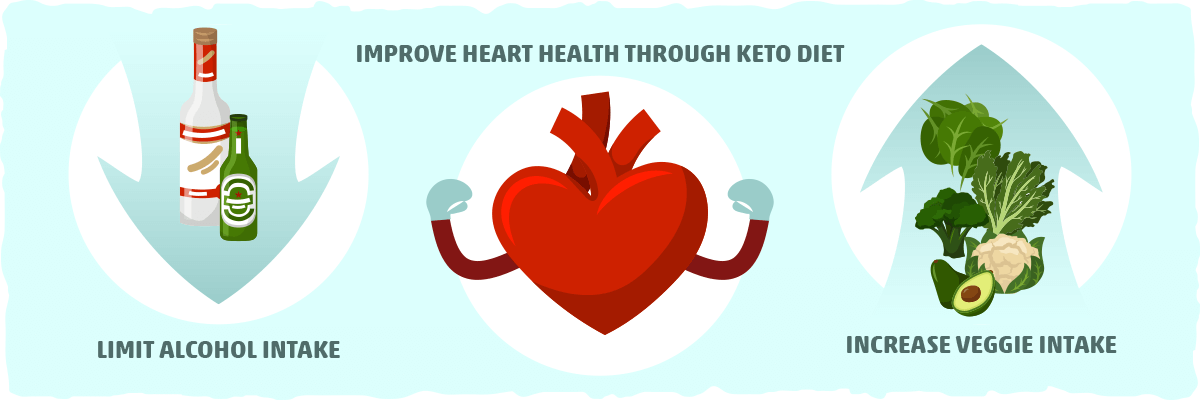
The toxic effects of alcohol and a poor quality diet will directly increase heart disease risk and drive the development of each one of the health issues mentioned above at the same time. Fortunately, the keto diet addresses diet quality and alcohol intake simultaneously by increasing the consumption of low-carb vegetables and limiting alcohol intake, so it doesn’t disrupt your efforts to get into ketosis.
Simply by adding more veggies in and taking the alcohol out, you’ll find it much easier to lose fat consistently as your blood lipids, blood sugar, and blood pressure all naturally improve. The keto diet will amplify these results for many people.
Putting It All Together – Can Keto Cause Heart Problems? Keto and Heart Disease Risk
The most accessible way to gauge the impact a diet has on heart disease is by seeing how it affects these six risk factors:
- Blood pressure
- Blood lipids
- Blood sugar
- Body fat levels
- Stress and other psychosocial factors
- Vegetable, fruit, and alcohol intake
If a specific diet is able to improve each one of these factors significantly, then it is reasonable to assume that the diet is a good option for preventing heart disease and reducing the risk of stroke and heart attack.
Does the keto diet stand up to the test? Overall, the current research literature indicates that the keto diet can improve each one of these risk factors for most people. This means that keto can be a heart-healthy option for those looking to reduce heart disease risk.
The only exception seems to be for those who have hypothyroid-related issues, familial hypercholesterolemia, and/or food allergies, food sensitivities, or mental health conditions that don’t respond well to the standard keto diet. People who fit into these groups should approach keto dieting with caution and may benefit from other diets that have been proven to reduce heart disease risk.
This brings us to another critical question: What is the best diet for heart disease?
Keto vs. The Mediterranean Diet for Heart Disease
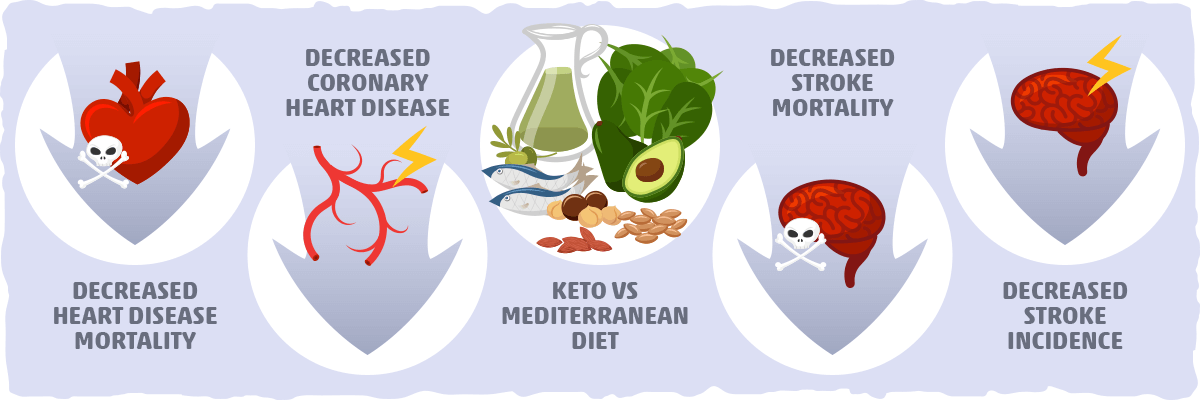
Although it isn’t explicitly stated, the consensus seems to be in favor of the Mediterranean diet as being the best option for people at high risk for heart disease. Even the American Heart Association’s dietary recommendations are almost identical to the Mediterranean diet.
The research also backs up the effectiveness of this approach. For example, a recent meta-analysis on the effect of the Mediterranean diet on the prevention of cardiovascular disease incidence and mortality found a few remarkable associations:
- Decreased heart disease mortality
- Reduced incidence of coronary heart disease
- Decreased stroke incidence
- Decreased stroke mortality
- Decreased heart attack incidence
These associations were put to the test in a large clinical trial as well. In this study, high-risk subjects who followed a Mediterranean diet supplemented with extra-virgin olive oil or nuts experienced a slightly reduced incidence of major cardiovascular events compared to a control reduced-fat diet.
Unfortunately, we don’t have sufficient data to directly compare the impact that Mediterranean diets and keto diets have on heart disease. Similar studies on heart disease incidence and mortality prevention have not been conducted on keto diets, and very few studies use both diets as an intervention.
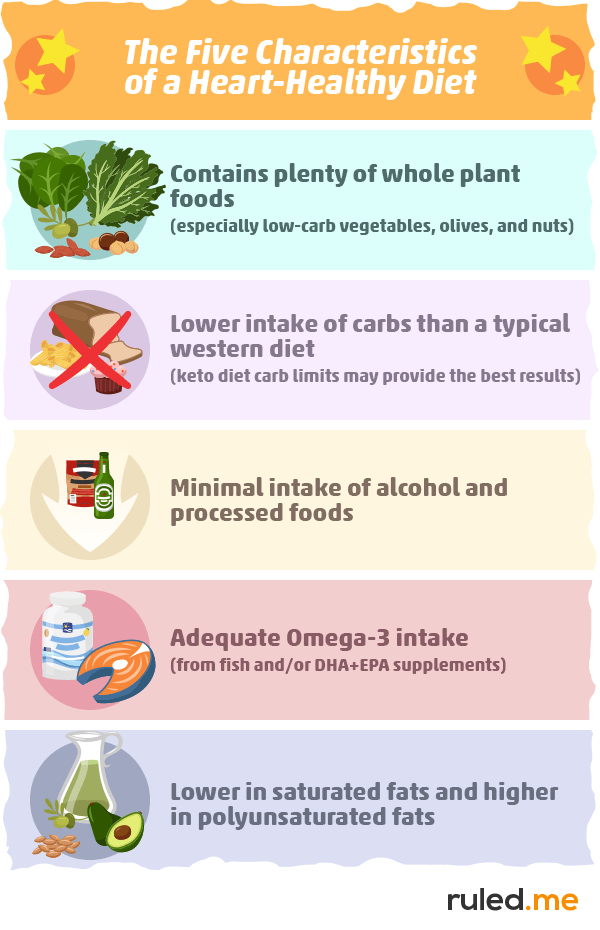
What Would The Best Diet for Heart Disease Look Like?
Currently, the data suggests that the Mediterranean diet is the safest and most effective option for the prevention of heart disease and its complications. Although the keto diet can significantly improve several risk factors for heart disease, research has yet to study its effects on heart disease as vigorously as the Mediterranean diet.
With the current data, however, we can make a few reasonable speculations as to what the ideal diet for preventing and potentially reversing heart disease would look like:
- Adequate intake of plant foods (especially low-carb vegetables, olives, and nuts).
- Lower in carbs than the typical western diet.
- Minimal consumption of alcohol and processed foods.
- Adequate fish intake (to increase omega-3 consumption).
- Lower in saturated fats and higher in polyunsaturated fats.
These seem to be the five essential characteristics behind the positive impact that the keto diet and Mediterranean diet can have on heart disease and its risk factors. Interestingly enough, research has already been done on this unique hybrid of the two diets to determine its effects on various aspects of health.
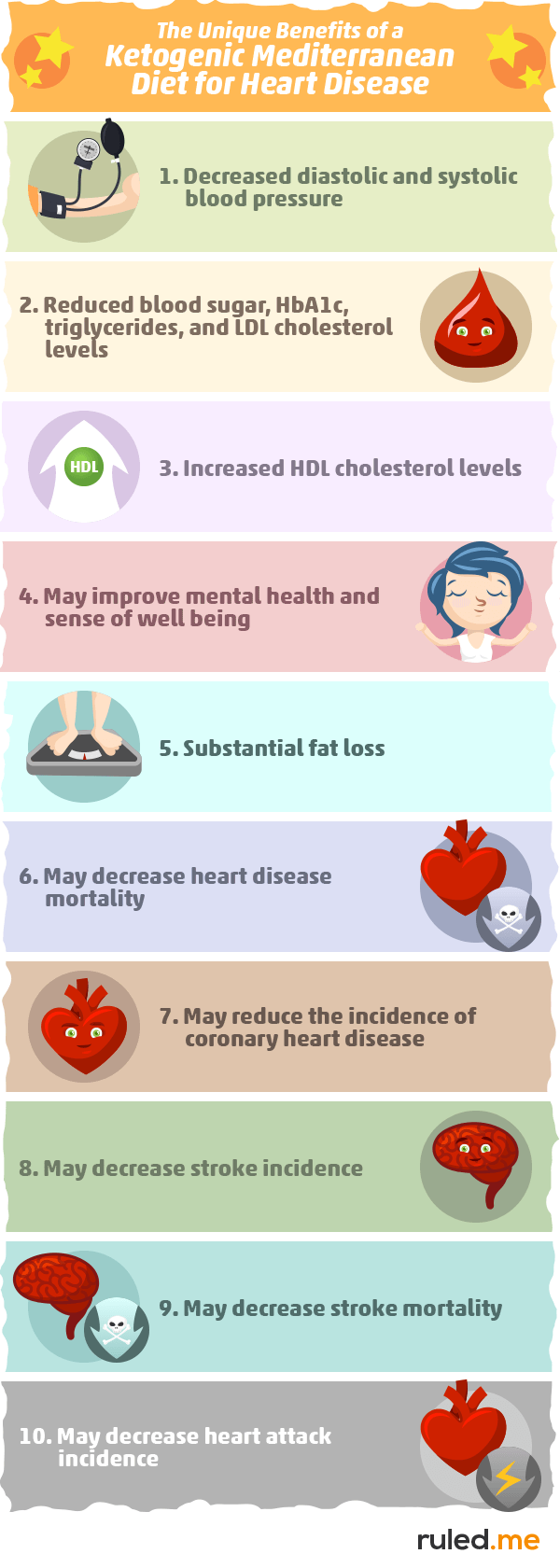
To summarize, feel free to reference the graphic below:
The Ketogenic Mediterranean Diet For Weight Loss and Heart Disease Prevention
In the first study, the researchers used a keto and Mediterranean diet combination they called a “Spanish Ketogenic Mediterranean Diet.” This diet included:
- Virgin olive oil as the principal source of fat (≥30 ml/day).
- Moderate red wine intake (200–400 ml/day).
- Green vegetables and salads as the primary source of carbohydrates.
- Fish as the main source of protein.
- Unlimited calories.
In other words, this was like a less strict keto diet with a strong bias toward olive oil, fish, and low-carb vegetables.
After 12 weeks of the following this diet, the results are what you’d expect from a typical keto diet, with significant decreases in body weight, blood pressure, glucose, and triglycerides. The most noteworthy finding, however, was what happened to each subject’s cholesterol numbers.
On average, there was a reduction in LDL cholesterol (114.52 mg/dl→105.95 mg/dl) and an increase in HDL cholesterol (50.10 mg/dl→54.57 mg/dl). This means that following a Mediterranean keto diet may improve cholesterol levels even more than the standard keto diet.
Similar results were found after six weeks of a Mediterranean ketogenic diet with the addition of herbal extracts. Significant reductions in total cholesterol (204 mg/dl to 181 mg/dl) and LDL cholesterol (150 mg/dl to 136 mg/dl) were noted, as well as an increase in HDL cholesterol (46 mg/dl to 52 mg/dl). Perhaps the increased antioxidant content of this diet from the herbal extracts lead to a more significant improvement in cholesterol levels.
One long-term study was also conducted comparing the effects of the Mediterranean keto diet with and without omega-3 supplementation. After 12-months, the researchers found significant decreases in total cholesterol, LDL cholesterol, and glucose levels for both groups. The omega-3 supplementation yielded greater decreases in triglycerides, insulin, and inflammatory cytokine levels.
The final trial worth highlighting is one that examined the effects of a diet that alternates between a non-keto and keto Mediterranean diet. In this study, obese subjects followed a staged diet protocol over a period of 12 months:
- Stage 1: 20 days of a Mediterranean keto diet
- Stage 2: 20 days low carb, non-ketogenic diet
- Stage 3: 4 months of a normal Mediterranean diet
- Stage 4: Another 20-day Mediterranean ketogenic diet phase
- Stage 5: 6 months of a normal Mediterranean diet
The result of this staged protocol were significant and stable decreases in total cholesterol, LDL cholesterol, triglycerides, and glucose levels after 12 months. HDL cholesterol showed small increases after the ketogenic phases, but after the full study period, there was no significant change (this is likely the result of increased carb consumption after the keto phase).
Also worth noting is that this alternating diet approach seemed to increase compliance, with only 8 of the 89 subjects failing to comply. This means that alternating between a keto and non-keto Mediterranean diet may be a more suitable option for those struggle to stay on a Mediterranean keto diet for the long-term.
Key Takeaways: What is the Best Diet for Heart Disease?
The current evidence is leaning toward a Mediterranean keto diet as being an ideal diet for addressing the many common risk factors for heart disease and its complications. This approach seems to provide us with all of the benefits of the keto diet and Mediterranean diet for heart health in one simple diet.
However, no studies have been done on cardiovascular disease incidence and mortality after following the Mediterranean keto diet, so it is difficult to determine if Mediterranean keto is any better or worse than the normal Mediterranean diet.
That being said, it is reasonable to speculate that a ketogenic version of the Mediterranean diet may have an edge over a normal Mediterranean diet because of the potential added benefits of decreasing carb intake and increasing ketone use. To learn more about this, you can follow our guide to the Ketogenic Mediterranean Diet.
Practical Applications: What Should You Do with Your Diet to Help Prevent Heart Disease?
There are various diet approaches you can use to prevent (and potentially reverse) heart disease. Research indicates that a diet with these characteristics is the best for your heart:
- Plenty of whole plant foods (especially low-carb vegetables, olives, and nuts).
- Lower intake of carbs than a typical western diet. Restricting carbs to the point of following a keto diet may help improve triglycerides, blood sugar, cholesterol, and body composition more than higher-carb diets.
- Minimal intake of alcohol and processed foods.
- Adequate omega-3 intake (from fish and/or DHA+EPA supplements).
- Lower in saturated fats and higher in polyunsaturated fats. Think olive oil instead of butter.
This diet approach is likely to provide you with the benefits of both the keto diet and the Mediterranean diet such as:
- Decreased diastolic and systolic blood pressure
- Reduced blood sugar, triglycerides, and LDL cholesterol levels
- Increased HDL cholesterol
- Optimized overall cholesterol levels
- Improved stress levels and sense of well being
- Substantial fat loss
- Decreased heart disease mortality
- Reduced incidence of coronary heart disease
- Decreased stroke incidence
- Decreased stroke mortality
- Decreased heart attack incidence
With any diet change, however, make sure you are monitoring your health and following an approach that you can turn into a heart-healthy lifestyle. Those with familial hypercholesterolemia and/or hypothyroid issues, in particular, need to be especially cautious with low-carb, high-fat eating.
Give the diet a try for at least a month and monitor your health throughout the process. If you find the Mediterranean keto diet is not improving your health and well being, then a non-keto Mediterranean diet with more high-carb plant foods may be a better option.
To help you get started, check out our comprehensive article on the Mediterranean Ketogenic Diet.
Sources
- Cardiovascular diseases (CVDs) – WHO
- HDL, Atherosclerosis, and Emerging Therapies — NCBI
- Modification of low density lipoprotein by endothelial cells involves lipid peroxidation and degradation of low density lipoprotein phospholipids — NCBI
- Statin Adverse Effects: A Review of the Literature and Evidence for a Mitochondrial Mechanism — NCBI
- Cholesterol, inflammation and innate immunity — NCBI
- The Total-to-HDL Cholesterol Ratio — What Does It Mean? — Chris Masterjohn PhD
- Effects of Thyroid Dysfunction on Lipid Profile — NCBI
- Dietary Guidelines to Treat and Prevent Atherosclerosis — PCRM
- When does atherosclerosis become irreversible? Chronological change from an early to an advanced atherosclerotic lesion observed by angioscopy. — NCBI
- Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis – The Lancet Public Health
- Low-carbohydrate diets and all-cause and cause-specific mortality: Two cohort Studies – NCBI
- The Global Burden of Cardiovascular Disease – SAGE Journals
- Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. – The Lancet
- Mediterranean diet, cardiovascular disease and mortality in diabetes: A systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. – NCBI
- The American Heart Association’s Diet and Lifestyle Recommendations – Heart
- Effects of Ketogenic Diets on Cardiovascular Risk Factors: Evidence from Animal and Human Studies – NCBI
- Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: an open label, non-randomized, controlled study – Cardiovascular Diabetology
- Dietary Intervention to Reverse Carotid Atherosclerosis – Circulation
- The National Cholesterol Education Program Diet vs a Diet Lower in Carbohydrates and Higher in Protein and Monounsaturated Fat: A Randomized Trial – JAMA Network
- Dietary patterns and the risk of major adverse cardiovascular events in a global study of high-risk patients with stable coronary heart disease – European Heart Journal
- Diet and Heart Disease—What Every Cardiologist Should Know – American College of Cardiology
- Long term successful weight loss with a combination biphasic ketogenic Mediterranean diet and Mediterranean diet maintenance protocol. – NCBI
- Effects of n-3 polyunsaturated fatty acids (ω-3) supplementation on some cardiovascular risk factors with a ketogenic Mediterranean diet. – NCBI
- Effect of ketogenic Mediterranean diet with phytoextracts and low carbohydrates/high-protein meals on weight, cardiovascular risk factors, body composition and diet compliance in Italian council employees. – NCBI
- Spanish Ketogenic Mediterranean diet: a healthy cardiovascular diet for weight loss – NCBI
- Coronary Heart Disease in Patients With Low LDL-Cholesterol – Circulation
- How Diabetes Drives Atherosclerosis – Science Daily
- Mechanisms of Plaque Formation and Rupture – Circulation Research
- Inflammation: The Common Pathway of Stress-Related Diseases – NCBI
- Psychological Stress and Cardiovascular Disease – NCBI
- Inflammation, Glutamate, and Glia: A Trio of Trouble in Mood Disorders – NCBI
- Atherosclerosis: Process, Indicators, Risk Factors and New Hopes – NCBI